Rejuvenate Your Fertility: The Ultimate Guide to PRP, Stem Cell, and Tissue Treatments for Ovarian Renewal
- Staff Writer
- Apr 22
- 11 min read
The Fundamentals of Cellular Aging
Our bodies operate through a continuous process of cellular renewal—young, healthy cells are generated while old, damaged cells are cleared away. This delicate balance maintains tissue function and overall health. However, as we age, this replenishment process becomes progressively less efficient.
"The aging process is actually an imbalance between cellular damage and cellular repair," explains Dr. Laura Niedernhofer, a researcher at the Institute on the Biology of Aging and Metabolism Department of Biochemistry at the University of Minnesota, Minneapolis. "What we're seeing in aging ovaries is not just depletion of eggs, but deterioration in the quality of the remaining follicles due to accumulated cellular damage and diminished repair mechanisms."
This fundamental aging process affects all tissues and organs, including the ovaries. In the reproductive system, this shifting balance is particularly significant since it directly impacts fertility potential and hormonal balance.
Understanding the Ovarian Aging Process
Normal Ovarian Function
The ovaries are central to female fertility, containing a finite number of follicles that each house an immature egg (oocyte). A woman is born with all the eggs she will ever have—approximately 1-2 million at birth—and this number steadily declines throughout her life. By puberty, around 300,000-400,000 follicles remain, and only about 400-500 will mature and be released during a woman's reproductive years.
It's crucial to understand that ovarian rejuvenation therapies cannot create new follicles or eggs. The goal of these treatments is to optimize the growth and development of existing follicles that might otherwise remain dormant or undergo atresia (cell death). These therapies aim to help the body release and develop more of the follicles a woman already has, improving both quantity and quality of available eggs.
"What we're doing with ovarian rejuvenation isn't creating new eggs—that's a misconception," clarifies Dr. Mary Everlane. "We're optimizing the environment of existing follicles, potentially reactivating dormant follicles, and improving the quality of eggs that develop from them."
Each month during the menstrual cycle, the body selects several follicles to begin development, but typically only one will reach full maturity and release an egg during ovulation. The rest undergo a process called atresia (cell death). This process accelerates with age.
The Aging Process
Several mechanisms contribute to ovarian aging. The continuous loss of follicles through atresia eventually leads to diminished ovarian reserve. Remaining eggs accumulate genetic and mitochondrial abnormalities with age. Aging ovaries experience decreased vascularization, limiting nutrient delivery. Accumulated damage from reactive oxygen species impairs cellular function. Additionally, altered follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels affect follicle development.
A 2022 study involving 510 women with poor ovarian response found that aging affects not just egg quantity but also quality, with "decreased fertilization and blastocyst formation rates and higher aneuploidy rates" in older patients.
Important Role of Growth Factors
Growth factors play a crucial role in ovarian function, influencing follicle recruitment and development, oocyte maturation, blood vessel formation (angiogenesis), cell proliferation and survival, and hormone production. As women age, the concentration and activity of these growth factors diminish, contributing to reduced ovarian function and fertility.
"Growth factors are essentially the body's natural signaling molecules that tell cells what to do—grow, divide, mature, or even die," explains Dr. Rebecca Wang, reproductive scientist at Fertility Partners Research Institute. "In aging ovaries, we see a dramatic reduction in both the production of these growth factors and the tissue's sensitivity to them."
As a result, a few ovarian rejuvenation options have evolved to improve the quantity and quality through triggering more growth factors in the ovary. Though not formally approved by the FDA, these options have shown encouraging results, albeit limitations.
Ovarian Rejuvenation Options
1. Platelet-Rich Plasma (PRP) Therapy
Scientific Basis
PRP is derived from the patient's own blood, which is processed to concentrate platelets. Platelets contain numerous growth factors stored in alpha granules, including Platelet-Derived Growth Factor (PDGF), Vascular Endothelial Growth Factor (VEGF), Transforming Growth Factor-beta (TGF-β), Epidermal Growth Factor (EGF), and Insulin-like Growth Factor-1 (IGF-1).
“Platelets as a main components of the PRP, contain more than 1100 different proteins, with numerous post-translational modifications, resulting in over 1500 protein-based bioactive factors” according to a paper published in 2016.
When injected into the ovaries, these growth factors may activate dormant follicles, improve blood flow, reduce inflammation, and potentially enhance ovarian function.
A 2022 systematic review and meta-analysis found that "PRP treatment resulted in higher antral follicle count, higher serum AMH, lower serum FSH, and a higher number of mature oocytes and embryos."
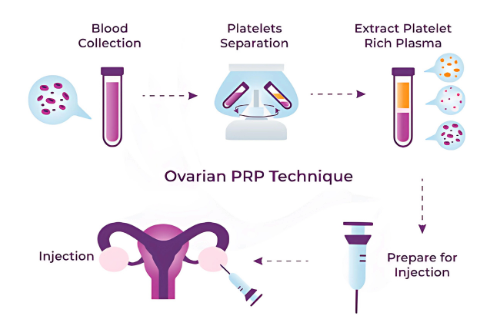
Procedure
The PRP procedure begins with blood collection, where 10-60ml of blood is drawn from the patient's arm. This blood is then processed through centrifugation to separate components and concentrate platelets (typically 2-5x normal concentration). The platelet-rich portion is extracted and sometimes calcium chloride or thrombin is added to activate platelets. The PRP is then injected directly into the ovaries using ultrasound guidance. The entire procedure takes approximately 60-90 minutes, and patients can usually resume normal activities within 24 hours.
"The PRP procedure is remarkably straightforward," says Dr. Jason Franasiak, reproductive endocrinologist at RMA New Jersey. "We draw blood, process it to concentrate the platelets, and inject it directly into the ovaries using the same ultrasound-guided approach we use for egg retrievals. Most patients experience minimal discomfort and can return to their normal activities the same day."
Frequency of Treatment
Due to its low risk profile and relatively quick procedure time, PRP treatment can be repeated regularly. The recommended baseline is every 3 months, but for patients undergoing frequent egg retrievals, monthly treatments may be considered to maximize follicular development. Treatment effects may last 3-12 months depending on individual response.
Pros and Cons
PRP therapy offers several advantages: it's a minimally invasive outpatient procedure that uses the patient's own blood products, minimizing risk of adverse reactions. It has a quick recovery time and can be repeated multiple times. There is growing evidence of effectiveness for certain patients, with potential improvements in both egg quality and quantity, as well as restoration of hormonal function in some cases. PRP is also compatible with other fertility treatments.
However, there are limitations to consider. Results vary significantly between individuals, and the procedure is still considered experimental in many countries. There is limited long-term data on effectiveness, and multiple treatments may be required. PRP is typically not covered by most insurance plans, and results may be temporary. Additionally, the procedure is not suitable for patients with certain blood disorders, and there is limited standardization of preparation methods.
Sarah M., a 38-year-old marketing executive who underwent PRP therapy, shares her experience: "After two failed IVF cycles with poor egg quality, I decided to try PRP. Three months after the procedure, my AMH level had increased from 0.8 to 1.3, and in my next retrieval, we got four high-quality embryos—a dramatic improvement from before. It wasn't a miracle cure, but it definitely made a significant difference for me."
2. Stem Cell Therapy
Scientific Basis
Stem cells are undifferentiated cells with the ability to develop into various specialized cell types. For ovarian rejuvenation, mesenchymal stem cells (MSCs) are most commonly used, which can be derived from bone marrow, adipose (fat) tissue, blood, or umbilical cord.
Research indicates that stem cells work through multiple mechanisms: they secrete growth factors and cytokines that support tissue regeneration (paracrine signaling), potentially develop into ovarian cells (direct differentiation), reduce inflammation and promote healing (immunomodulation), and stimulate new blood vessel formation (angiogenesis).
According to a 2022 study in the Journal of Translational Medicine, "Stem cells, which are characterized by their undifferentiated nature, self-renewal capability, and potential to differentiate into various cell types, have emerged as promising avenues for treating premature ovarian insufficiency."
Procedure
The stem cell procedure begins with harvesting, which varies depending on the source. Bone marrow is extracted from hip bone under local anesthesia; adipose tissue is collected via mini-liposuction procedure; or blood is drawn and processed to isolate specific stem cells. The cells are then isolated, purified, and sometimes expanded in a laboratory before being prepared in a solution for injection. Finally, they are delivered to the ovaries via ultrasound-guided injection. The complete process may take several hours to days depending on whether expansion is required, and recovery time varies based on harvesting method but is typically 1-3 days.
Dr. Livia Chen, stem cell researcher at the Institute for Regenerative Medicine, explains: "The most important aspect of stem cell therapy is ensuring we're using the right type of cells, at the optimal concentration, and delivering them properly. There's still a lot we're learning about the ideal parameters, but we're seeing encouraging results in selected patient populations."
Frequency of Treatment
Stem cell therapy is typically administered as a single treatment, with repeat treatments considered after 6-12 months based on response. Effects may last longer than PRP due to the self-renewing properties of stem cells, but are not as directly boosting the growth factors in the ovary as PRP does.
Pros and Cons
Stem cell therapy offers potential for longer-lasting effects than PRP and may provide more comprehensive tissue regeneration. It can deliver continuous production of growth factors over time and may address more severe cases of ovarian insufficiency. Growing research shows promising results for certain applications, and it can be combined with PRP for enhanced effects.
However, stem cell therapy involves a more invasive harvesting procedure than PRP and comes with a higher cost. It requires more complex processing requirements and faces greater regulatory restrictions in many countries. There is limited standardization across treatment centers and more potential risks than PRP therapy. Additionally, it has a longer recovery time than PRP and is still highly experimental with less clinical data than PRP.
3. Ovarian Tissue Cryopreservation and Transplantation
Scientific Basis
This approach involves surgically removing ovarian tissue when it's healthy, preserving it through freezing (cryopreservation), and later reimplanting it when needed. Unlike the other methods that aim to rejuvenate existing tissue, this preserves younger tissue for future use.
The transplanted tissue contains primordial follicles with immature eggs, ovarian stromal cells that provide structural support, growth factors naturally present in young ovarian tissue, and cells that produce hormones like estrogen and progesterone.
A systematic review reported that "over 78% of the patients who received fresh or frozen ovarian tissue showed ovarian function restoration and in over 58% of patients, pregnancies occurred."
Procedure
The ovarian tissue cryopreservation and transplantation process begins with tissue collection through laparoscopic surgery to remove part or all of one ovary. Typically the outer cortex is harvested, which contains the majority of follicles. The tissue is then processed by cutting it into thin strips (1-2mm thickness) and prepared with cryoprotectants to prevent ice crystal formation. It is then frozen using slow freezing or vitrification (rapid freezing) methods and stored in liquid nitrogen at -196°C, where it can be maintained for years or decades.
When needed, the tissue undergoes careful thawing protocol to maintain cell viability before surgical reimplantation, either orthotopically (placed back in the ovarian region) or heterotopically (placed in another location like abdominal wall). Recovery typically requires 1-2 weeks, and ovarian function may return within 3-6 months after transplantation.
Dr. Samuel Katz, Director of the Fertility Preservation Program at University Medical Center, comments: "Ovarian tissue cryopreservation is particularly valuable for young cancer patients who need to preserve fertility before undergoing gonadotoxic therapies."
Frequency of Treatment
Ovarian tissue cryopreservation is usually performed once for removal, but the tissue can be divided into portions for multiple transplantations over time. Transplanted tissue typically functions for 2-7 years before being depleted.
Recent data indicates that "more than 130 live births have been reported worldwide with the aid of cryopreserved ovarian tissue and the estimated birth rate is currently approximately 30%."
Pros and Cons
Ovarian tissue cryopreservation and transplantation preserves original, younger ovarian tissue with naturally occurring growth factors and can restore both fertility and hormonal function. It has resulted in over 130 live births worldwide and is not dependent on stimulating aging tissue. It can be performed before cancer treatments that might damage ovaries, may restore natural menstrual cycles, and allows potential for natural conception.
However, this approach requires two surgical procedures and carries a risk of reintroducing malignant cells if performed for cancer patients. It has limited availability and specialized centers, significant expense, and transplanted tissue has a limited lifespan. There is also a delay between transplantation and return of function, risk of tissue loss during freezing/thawing process, and it is not suitable for patients who already have severely diminished ovarian function.
The number of patients having gone through ovarian tissue transplantation is not significant enough to draw a conclusion of the risk and reward profile of this treatment. The success rate is also highly dependent on the surgeon performing the procedures. Therefore, it is the least recommended option of the three.
Role of Growth Factors in Each Approach
Growth Factors in PRP Therapy
PRP delivers an immediate, concentrated dose of multiple growth factors directly to the ovaries. These growth factors work as signaling molecules that activate cellular receptors on ovarian cells, trigger intracellular signaling cascades, stimulate dormant follicles to begin development, promote angiogenesis to improve blood flow, reduce cellular inflammation and oxidative stress, and support cellular survival pathways.
The advantage of PRP is the rapid availability of these growth factors, with the limitation being their relatively short half-life. This explains why repeat treatments are beneficial for maintaining the effect.
Growth Factors in Stem Cell Therapy
Stem cells act as "growth factor factories" that can continuously produce these signaling molecules. Their mechanisms include initial release of pre-stored growth factors, ongoing production of growth factors for extended periods, delivery of growth factors in physiologic concentrations, adapting growth factor production based on the local environment, direct cell-to-cell contact signaling, and potential replacement of damaged cells.
The advantage of stem cells is their ability to provide sustained growth factor release over longer periods, with the limitation being the more complex harvesting and preparation process. This indirect impact on the ovarian function might not be the most efficient for fertility purposes.
Growth Factors in Ovarian Tissue Transplantation
Transplanted ovarian tissue contains the natural architecture and cells already designed to produce appropriate growth factors: intact follicular units with their surrounding support cells, native growth factor producing cells in proper proportions, young cells with optimal growth factor production capacity, natural release patterns of growth factors, and complete ovarian microenvironment for optimal function.
The advantage of tissue transplantation is the preservation of the entire functioning system, with the limitation being the need for surgical procedures and the eventual depletion of the transplanted tissue.
Making an Informed Decision
Factors to Consider
When deciding which ovarian rejuvenation approach might be most appropriate, several factors should be considered. Current ovarian function plays a significant role — PRP may be suitable for mild to moderate diminished ovarian reserve, stem cells might be considered for more severe cases, and tissue transplantation requires prior preservation when ovarian function was better.
Age is another important factor. PRP shows better results in patients between age 35 and 42, but can be tried at any age. Stem cell therapy has shown some promise in older patients, while tissue transplantation is most effective when tissue was preserved at a young age.
Medical history, including previous cancers or risk of malignancy, autoimmune conditions, and blood disorders, may affect suitability for different approaches. Time frame is also important—PRP offers the quickest procedure and recovery, stem cell therapy requires more preparation time, and tissue transplantation has the longest lead time if tissue isn't already preserved.
Cost and accessibility vary among treatments. PRP is generally the most affordable and widely available option, stem cell therapy involves higher costs and specialized facilities, and tissue transplantation requires specialized centers and significant expense.
Goals should also guide decision-making, whether they involve improving egg quality for IVF, restoring natural fertility, addressing hormonal symptoms, or preserving fertility for future use.
Recommendation: Why PRP Is Often Preferred
When comparing the three approaches to ovarian rejuvenation, PRP therapy often emerges as the preferred option for many patients and practitioners for several key reasons.
First, the primary need in ovarian rejuvenation is for growth factors that can stimulate and optimize existing ovarian tissue. While stem cells offer both growth factors and potential cellular replacement, the growth factor aspect alone is often sufficient for most cases of diminished ovarian reserve. PRP delivers these essential growth factors directly and efficiently.
Second, PRP offers a favorable balance between clinical effectiveness and practical considerations such as procedure time, recovery, and cost. It can be seamlessly integrated into IVF treatment protocols, making it particularly suitable for women actively pursuing fertility treatments. Unlike more invasive options, PRP can be performed regularly with minimal risk, allowing for ongoing support of ovarian function.
Recommended Treatment Schedule
For optimal results with PRP therapy, a minimum recommendation is treatment every 3 months to maintain consistent levels of growth factors supporting ovarian function. For IVF patients, the ideal approach is to consider PRP treatment with each egg retrieval cycle. This timing is advantageous because the ovarian stimulation process creates a controlled form of stress that PRP can complement, the ultrasound-guided approach used in egg retrieval makes simultaneous PRP administration technically straightforward, the growth factors from PRP can help support recovery of the ovaries post-retrieval, and this coordinated timing may help optimize follicle development for subsequent cycles.
Frequency can be modified based on individual response, AMH levels, and clinical outcomes. Many reproductive specialists now suggest beginning with this approach before considering more invasive or expensive options like stem cell therapy or ovarian tissue transplantation.
Conclusion
Ovarian rejuvenation is an evolving field with promising options for women facing diminished ovarian reserve or premature ovarian insufficiency. Each approach offers distinct advantages based on individual circumstances and goals. Consulting with reproductive specialists experienced in these techniques is essential for determining the most appropriate treatment path.
While these treatments show promise, they should be approached with realistic expectations, understanding that results vary significantly between individuals. The field continues to advance, with ongoing research likely to refine and enhance these techniques in the coming years.




Comments