The Paradoxical Pill: Why Doctors Prescribe Birth Control Before IVF
- Michelle Lim
- Apr 16
- 6 min read
When Sarah Williams was preparing to start her first IVF cycle, she was surprised by her doctor's initial prescription: birth control pills. "It seemed completely counterintuitive," says Williams, a 36-year-old marketing executive. "I had spent years trying not to get pregnant, and now that I wanted a baby, I was back on the pill."
Williams isn't alone in her confusion. Nearly 60% of all IVF cycles in the United States begin with a course of hormonal contraception, according to fertility clinic data – a practice that might seem paradoxical but is supported by significant clinical evidence and endorsed by the American Society for Reproductive Medicine (ASRM).
"It's one of the most common misconceptions patients have about IVF," explains Dr. Jessica Martinez, a reproductive endocrinologist at Pacific Fertility Center. "The pill isn't being used for contraception in this context – it's a powerful tool that helps us create optimal conditions for IVF."

The Science Behind the Strategy
Birth control pills serve several crucial functions when used before IVF treatment. A 2024 ASRM committee opinion states that "the use of hormonal contraception can be considered to aid in the timing of ART cycles, reduce the risk of ovarian cysts at IVF cycle initiation, and optimize visualization before hysteroscopy."
Creating a Clean Hormonal Slate
When fertility specialists discuss "quieting the ovaries" before stimulation, they're referring to a specific hormonal environment that improves treatment outcomes.
"We're looking for very specific hormone levels at the start of stimulation," says Dr. Robert Chen, an IVF laboratory director at Northeast Reproductive Medicine. "Ideally, we want estradiol below 50 pg/mL, FSH under 10 mIU/mL, and LH less than 10 mIU/mL. Birth control helps create this baseline consistently."
This hormonal reset allows doctors to more precisely calculate medication doses and predict how the ovaries will respond to stimulation. According to Dr. Chen, patients starting from this standardized baseline typically show more uniform follicular development during stimulation.
Synchronizing Follicular Development
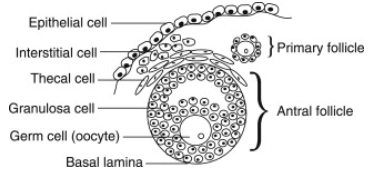
One of the most significant benefits of birth control pretreatment is the synchronization of ovarian follicles – the fluid-filled sacs containing immature eggs.
"In a natural cycle, follicles develop at varying rates, with one becoming dominant," explains Dr. Sophia Lin, a reproductive endocrinologist specializing in PCOS. "Birth control temporarily suppresses all follicular development, allowing existing follicles to regress to a similar early developmental stage."
When stimulation begins after this synchronization, the goal is to have multiple follicles grow at a similar rate. Fertility specialists typically look for follicles measuring 2-8mm in diameter at baseline, with no dominant follicles larger than 10mm.
Jennifer Cohen, a 34-year-old teacher who underwent IVF last year, credits this approach with her successful egg retrieval. "My first cycle without birth control yielded only three mature eggs," she recalls. "After using birth control before my second cycle, we retrieved eight mature eggs, because they were growing at similar pace and size."
Preventing Ovarian Cysts
Functional ovarian cysts – which develop during natural menstrual cycles – can interfere with stimulation medications and even lead to cycle cancellation. Research shows that birth control significantly reduces the risk of new cysts forming.
A study cited in the ASRM document found that the incidence of ovarian cysts in women not using contraception was 9.5% compared to just 2.4% in women who had been on hormonal contraception for at least three months.
"One common misconception is that birth control helps resolve existing cysts," notes Dr. Martinez. "The evidence actually shows it's more effective at preventing new cysts from forming rather than shrinking existing ones."
In fact, a comprehensive Cochrane Review examined eight randomized controlled trials comparing birth control to expectant management for treating existing cysts. The review found no evidence that birth control pills speed up cyst resolution. Most functional cysts resolve spontaneously within 3-6 weeks regardless of treatment approach. Cysts that persist beyond this timeframe are often pathologic (like endometriomas or dermoid cysts) rather than functional.
"If a patient comes in with an existing cyst, we typically wait for it to resolve naturally rather than prescribing birth control to treat it," explains Dr. Martinez. "However, we often recommend birth control to prevent new cysts from developing in future cycles."
Scheduling Benefits
For both patients and clinics, the scheduling flexibility provided by birth control pretreatment is invaluable.
"Before my IVF cycle, I had an important conference I couldn't miss," says Williams. "Using birth control allowed my doctor to time my egg retrieval for the following week when my schedule was clear."
Many fertility clinics use birth control to "batch" IVF cycles – coordinating several patients to undergo treatment simultaneously, which improves laboratory efficiency. It's also essential for third-party reproductive arrangements, helping synchronize egg donors with recipients.
Personalizing Protocols for Different Patients
While birth control pretreatment is common, approaches vary significantly based on individual patient factors.
Special Considerations for PCOS
For patients with polycystic ovary syndrome (PCOS), birth control can provide additional benefits beyond synchronization.
"PCOS patients often have elevated LH levels and excess androgens, which can lead to erratic responses during stimulation," says Dr. Lin. "Pretreatment can help regulate these hormones and potentially reduce the risk of ovarian hyperstimulation syndrome."
Research on PCOS patients has shown mixed results. Some studies found improved implantation and clinical pregnancy rates with at least three months of pretreatment, while others showed potential adverse effects on live birth rates after fresh embryo transfers with shorter durations (21-25 days) of pretreatment.
Benefits for Endometriosis Patients
Women with endometriosis may see particular benefits from birth control pretreatment. According to the ASRM document, one study showed that a 6-8 week course of hormonal contraception in women with endometriosis resulted in higher pregnancy rates per retrieval (35% versus 12.9%) compared to controls.
"Endometriosis creates an inflammatory environment that can impair both egg quality and embryo implantation," explains Dr. James Wilson, who specializes in treating reproductive disorders. "Suppressing this inflammation with hormonal contraception before IVF appears to create more favorable conditions."
Type of Birth Control Matters
Not all birth control formulations affect ovarian stimulation in the same way. Some research suggests that the progestin component may influence outcomes.
"Birth control pills contain synthetic versions of the female hormone progesterone (called 'progestins'). Different generations of these synthetic hormones have been developed over time, with newer versions generally designed to have fewer side effects," explains Dr. Wilson.
One small study found egg donors on birth control pills with testosterone-like effects had significantly lower egg yields (11.3 versus 16.6 eggs) than those without pretreatment.
However, the ASRM committee noted that a recent retrospective analysis found no significant difference in clinical pregnancy or live birth rates between women using different generations of progestins, suggesting more research is needed.
Impact on Ovarian Reserve Testing
Women planning fertility treatment should be aware that hormonal contraception can temporarily affect tests used to assess ovarian reserve.
"Both antimüllerian hormone (AMH) levels and antral follicle count can be suppressed by approximately 30% with long-term hormonal contraception," explains Dr. Martinez. "This effect is particularly notable in women who have used birth control for more than six months."
After stopping contraception, these markers typically begin to increase within one month and plateau after about six months. Approximately 80% of women show an increase in antral follicle count after stopping hormonal contraception, with this effect being more pronounced in women with initially low counts.
For this reason, fertility specialists often recommend ceasing birth control 2-3 months before diagnostic testing to ensure accurate assessment of ovarian reserve.
Practical Considerations for Patients
Most patients take birth control pills for 2-4 weeks before beginning injectable fertility medications, though the exact protocol varies based on individual factors and clinic preferences.
The process typically involves:
Taking birth control pills for 2-4 weeks
Stopping pills and waiting 2-5 days for withdrawal bleeding
Baseline ultrasound and bloodwork on day 2-3 of bleeding
Starting stimulation medications if hormone levels are optimal
Patients should be aware that pretreatment with birth control might increase the amount of stimulation medication needed. A meta-analysis showed that women with birth control pretreatment required significantly higher gonadotropin doses (+542 IU on average) and longer stimulation periods (+1.41 days) compared to those without pretreatment.
"This doesn't typically affect outcomes in terms of egg quality or pregnancy rates," says Dr. Chen, "but it's something patients should know when planning for medication costs."
Questions to Ask Your Doctor
If you're considering IVF and your doctor recommends birth control pretreatment, consider asking:
Which type of birth control is best for my specific situation?
How long will I need to take it before starting stimulation?
Will this affect the amount of medication I'll need?
Are there any risks or side effects I should be aware of?
Based on my diagnosis, are there advantages to using or avoiding birth control?
How will this impact my treatment timeline?
It's also important to discuss any contraindications to hormonal contraception, such as a history of migraines with aura, increased risk of venous thromboembolism, or cardiovascular disease.
The Future of Pretreatment Protocols
As reproductive medicine continues to advance, protocols for IVF preparation are becoming increasingly personalized.
"We're moving away from one-size-fits-all approaches," says Dr. Martinez. "The future lies in tailoring protocols to each patient's specific hormonal profile, diagnosis, and treatment goals."
For Williams, whose IVF journey resulted in the birth of her daughter last year, the initial confusion about birth control quickly gave way to appreciation for the science-based approach.
"In retrospect, I'm grateful for that month on birth control," she says. "It seems to have given my body the reset it needed before the stimulation process. The whole experience taught me that fertility treatment is often counterintuitive but incredibly precise."
This article is for informational purposes only and does not constitute medical advice. Always consult with a healthcare provider regarding your specific situation.



Comments