Double Your Eggs in One IVF Cycle: How Luteal Phase Retrieval Transforms IVF Results
- Michelle Lim
- Apr 27, 2025
- 4 min read
When Sarah first heard about luteal phase egg retrieval during her fertility consultation, she was both intrigued and confused. After three conventional IVF cycles with disappointing egg yields, her reproductive endocrinologist suggested trying the "Shanghai protocol," also known as DuoStim. As someone who had already invested significant time, money, and emotional energy into fertility treatments, the prospect of potentially doubling her egg yield in a single menstrual cycle seemed almost too good to be true.
The IVF Challenge: Why Traditional Protocols Were Failing Her
Sarah's fertility journey had followed the standard playbook until that point. Each cycle began with medications on day 2 or 3 of her period to stimulate her ovaries during the follicular phase, followed by monitoring appointments to track follicle growth. When her lead follicles reached around 18mm, she'd receive a trigger shot to mature the eggs before retrieval about 36 hours later.
The problem? Despite good follicle counts at the beginning of each cycle, Sarah would end up with only 3-4 mature eggs at retrieval. Her doctor explained that while she'd have 10-12 follicles visible on ultrasound, only the larger ones would respond to the trigger shot. The smaller follicles (particularly those under 10mm in diameter), which hadn't yet developed sufficient LH receptors, would not respond to the trigger. These smaller follicles would then undergo atresia—a natural degradation process—and would simply be lost when her next period arrived.
The Luteal Phase Retrieval Protocol Breakthrough: Rescuing Follicles Others Discard
Before agreeing to the procedure, Sarah needed to understand how it worked. Her doctor explained that traditionally, fertility specialists believed that egg development only occurred during the follicular phase. However, researchers in Shanghai discovered that a second wave of follicular development could be stimulated during the luteal phase – the part of the menstrual cycle after ovulation.
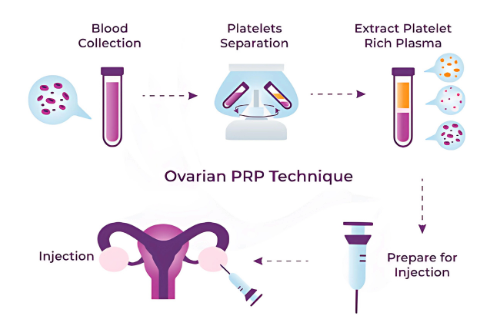
The protocol would involve:
A regular follicular phase stimulation and egg retrieval
Using Lupron as the trigger shot instead of hCG
Starting a second round of stimulation medications immediately after the first retrieval
A second egg retrieval about 10 days later, still within the same cycle

The Lupron trigger was particularly important because it causes a surge in both LH and FSH. While the LH would trigger maturation in her larger follicles (typically those over 10mm), the FSH boost would give the smaller follicles a head start for the second round of stimulation.
Her doctor explained that in conventional IVF, the fate of those smaller follicles (under 10mm) is predetermined – they simply don't have enough LH receptors to respond to the trigger shot. Without intervention, these immature follicles would undergo atresia (cellular death) during the luteal phase, and the body would eliminate them during the next menstrual period. It's a completely natural process, but in the context of IVF, it represents lost potential – eggs that could have potentially developed into viable embryos.
9 Eggs Instead of 4: How DuoStim More Than Doubled Her Chances
Sarah won't sugarcoat it – doing two stimulation cycles back-to-back was intense. After her first retrieval (which yielded 4 mature eggs), she barely had time to recover before starting injections again. The monitoring appointments continued, and she watched with amazement as those smaller follicles – the ones that would have undergone atresia in a conventional cycle – began to grow.
Her doctor explained the fascinating physiology at work: During the follicular phase retrieval, follicles smaller than 10mm hadn't developed enough LH receptors to respond to the Lupron trigger. However, the FSH component of the Lupron trigger gave these smaller follicles just enough stimulation to keep them viable instead of immediately entering atresia. Then, with the second round of stimulation medications, these follicles continued developing receptors and growing to maturity during the luteal phase, when they would normally be programmed to die off.
The second retrieval felt like a bonus round. Sarah went into the procedure with managed expectations, but emerged with 5 additional mature eggs – more than doubling her total from a single menstrual cycle.
What surprised her most was that the quality of the eggs from her luteal phase retrieval was comparable to those from the follicular phase. When fertilized, they developed into embryos at similar rates. Her doctor explained that once follicles reach maturity, regardless of which phase they matured in, their eggs have similar developmental potential.
Is Luteal Phase Retrieval Right for Everyone?
Sarah's experience with luteal phase retrieval gave her more embryos to work with than any previous cycle, but it's not necessarily the right approach for everyone. The protocol is particularly beneficial for those with:
Poor response to conventional stimulation
Diminished ovarian reserve
Limited time for fertility preservation (such as before cancer treatment)
Advanced maternal age
The downside? It's physically and emotionally demanding to undergo two retrievals so close together. The medication costs are also higher, and not all insurance plans cover this approach.
The Takeaway: Questioning Conventional Wisdom
Sarah's journey with luteal phase egg retrieval taught her that reproductive medicine continues to evolve, challenging long-held assumptions about how our bodies work. Those small follicles that would have been lost with her period instead gave her five more chances at pregnancy.
For those struggling with conventional IVF protocols, asking about luteal phase stimulation might open up new possibilities. While it's not a miracle solution, it represents one more tool in the growing arsenal of fertility treatments – and sometimes, those extra eggs can make all the difference.



Comments